NFCR Fellow’s Research Sheds Light on Mechanism for Blood Vessel Formation in Cancer
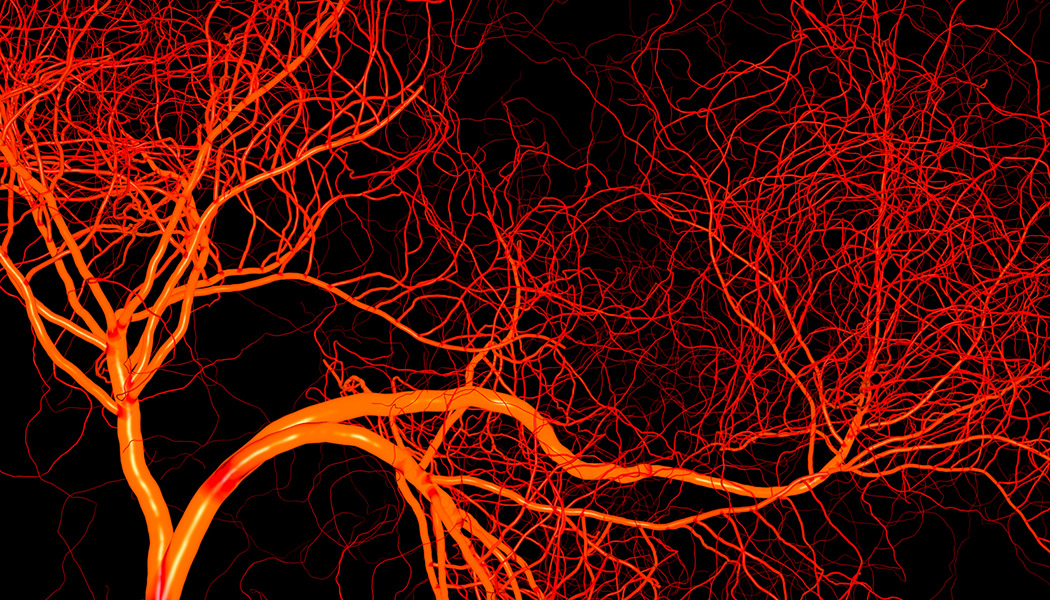
Dr. Xiang-Lei Yang, and NFCR-funded scientist Dr. Paul Schimmel, are worldwide experts in aminoacyl-tRNA synthetases (aaRS). aaRS is a family of enzymes that catalyze the synthesis of proteins from tRNA. While aaRS’s are best known for their role in protein synthesis, Dr. Yang discovered that a particular aaRS, SerRS, also plays a role in inhibiting angiogenesis.
Prior angiogenesis research suggests that two genes — c-Myc and HIF-1 — are responsible for promoting blood vessel growth in healthy cells and tumors alike. As such, the turning on and transcription of these genes can promote tumor oxygenation and growth. In particular, c-Myc is one of the most important cancer-causing genes upregulated in many types of cancer. It also controls the gene for the production of VEGF, a blood vessel growth factor.
In addition to its role in protein synthesis, SerRS limits blood vessel growth by inhibiting the function of the c-Myc and HIF-1. In the study published in PLOS Biology (December 2020), Yang and her fellow researchers share the discovery that during hypoxia, or oxygen starvation, proteins known as ATM/ATR are activated. The ATM/ATR protein activation “silences” or inhibits SerRS and promotes the formation of new blood vessels. Additionally, in separate studies of mice and human breast tissue, the researchers were able to display that ATM/ATR activation had a blocking effect on SerRS and resulted in reduced tumor size.
In researching the role of ATM/ATR activation, and SerRS in breast cancer, Dr. Yang’s team found that the expression of SerRS is positively correlated with a greater rate of survival in breast cancer patients. Also, SerRS is significantly downregulated when metastasis, or cancer spread, occurs. Similar findings have been made in several other cancer types including brain, esophageal, kidney (clear cell), rectal, stomach, and thyroid cancers. These findings suggest that SerRS can inhibit the growth and metastasis of certain cancers and that ATM/ATR activation can counter that inhibition.
These discoveries, funded in part by the National Foundation for Cancer Research, are core to our understanding of why and how tumors form new blood vessels and metastasize. As such, these discoveries may lead to novel therapeutic approaches that seek to limit ATM/ATR activation.
A world without cancer is possible. Help us turn lab breakthroughs into life-saving realities.

5.7 Million+
Donors who have fueled NFCR’s mission

$420 Million+
Invested in high-impact research & programs

36+ Labs & Hundreds of
Nobel Laureates & Key Scientists received NFCR funding, driving breakthrough research