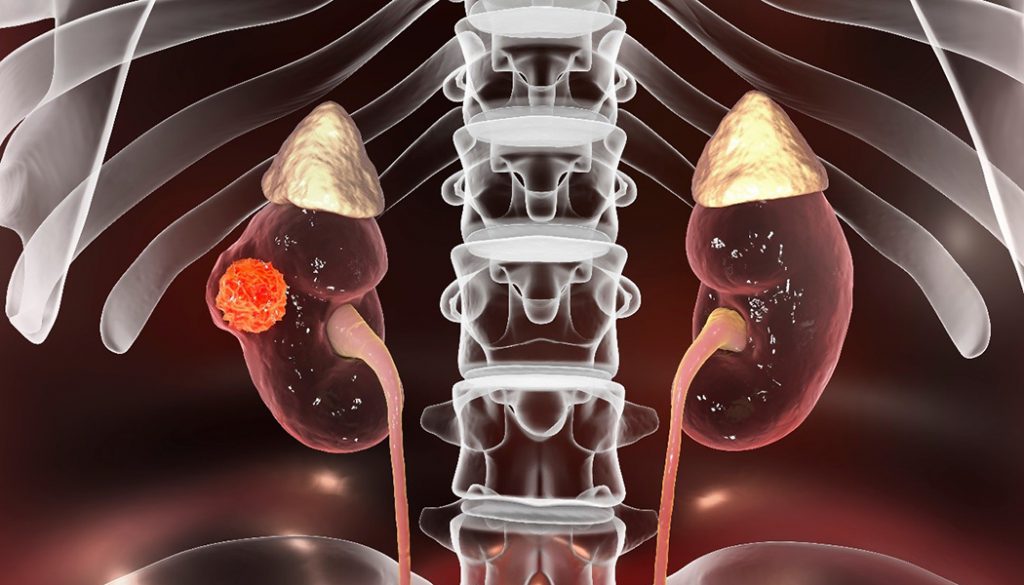
Kidney Cancer
Kidney cancer is among the 10 most common cancers in both men and women. While the rate of people being diagnosed with kidney cancer has been slowly increasing since the 1990s, in part due to increased use of medical imaging, the death rate has been slowly declining since the middle of the 1990s.
Key Facts
- An estimated 81,800 new cases of kidney cancer will be diagnosed in the U.S. in 2023, with 14,890 deaths expected to result from the diagnosis.
- The lifetime risk for developing kidney cancer is about 1 in 44 in men and 1 in 75 in women.
- Men are twice as likely to develop kidney cancer as women.
- Kidney cancer is uncommon in people younger than 45 and the average age of people when they are diagnosed is 64.
- The overall five-year survival rate for people with kidney cancer is 77%.
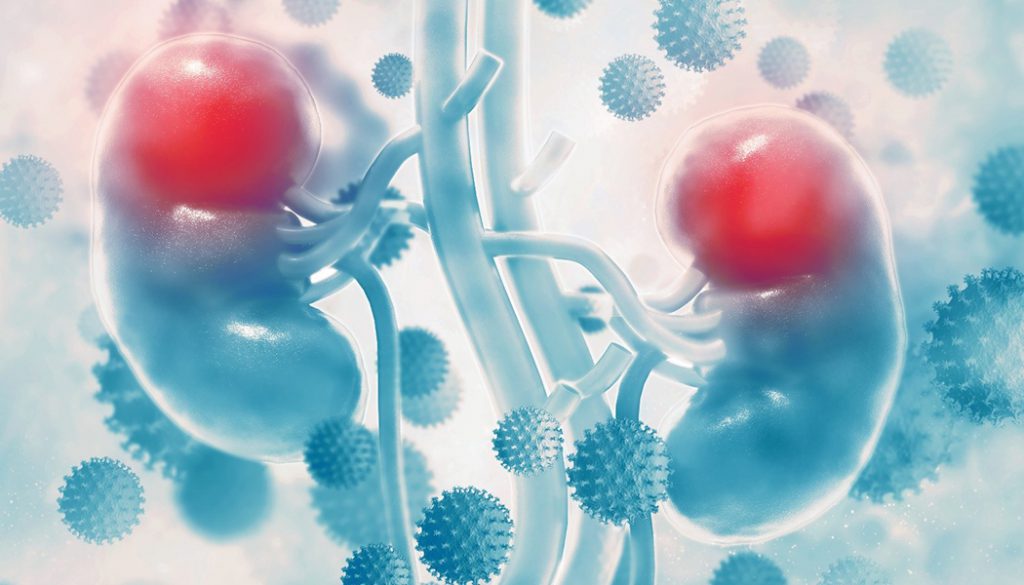
- Risk factors include smoking, obesity, high blood pressure, family history of kidney cancer, advanced or chronic kidney disease, and exposure to radiation therapy or carcinogenic chemicals such as trichloroethylene. African Americans and American Indians/Alaska Natives have slightly higher rates of renal cell carcinoma (most common type of kidney cancer) than do Caucasians.
Source: American Cancer Society’s Cancer Facts & Figures 2023 and the Society’s website
Signs and Symptoms
A symptom is a change in the body that a person can see and/or feel. A sign is a change that the doctor sees during an examination or on a laboratory test result. If you have any of the symptoms below, it does not mean you have cancer but you should see your doctor or health care professional so that the cause can be found and treated, if needed.
- Blood in the urine
- Low back pain on one side (not caused by injury)
- A mass (lump) on the side or lower back
- Fatigue (tiredness)
- Loss of appetite
- Weight loss not caused by dieting
- Fever that is not caused by an infection and that doesn’t go away
- Anemia (low red blood cell counts)
- swelling of the ankles and legs
- high blood pressure
- For men, rapid development of enlarged veins around a testicle (particularly the right testicle)
Source: American Cancer 2023 and American Society of Clinical Oncology Cancer.net 2021


Kidney Cancer Awareness Month is recognized in March. To help accelerate cures please make a gift today.