Immunotherapy
What is Immunotherapy?
The immune system is the body’s defense against disease as it recognizes and destroys any foreign material that could cause harm. In some instances, the immune system can recognize cancer cells as abnormal and kill them; in others, the cancer evades the immune system wreaking havoc in our bodies.
In recent years, some of the most promising advances in cancer research involve immunotherapies – treatments that use the immune system to fight diseases like cancer. By finding new ways to help the immune system recognize cancer cells – specifically in solid tumors, and strengthen its response to destroy them, researchers are looking for long-lasting solutions to cure cancer.
Support Breakthroughs in Immunotherapy Cancer Research and Beyond.
Related Content
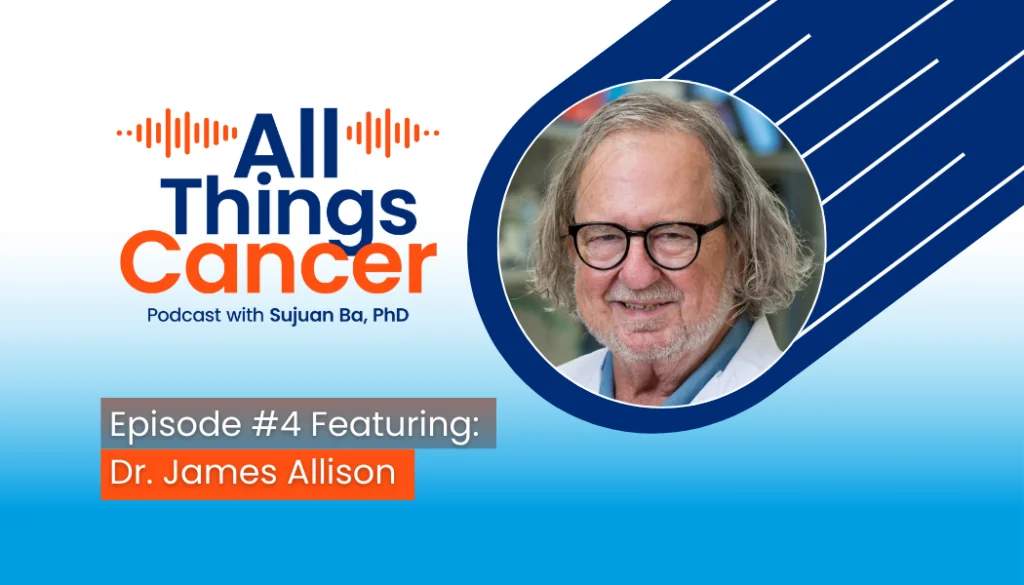
All Things Cancer Episode #4: Dr. James Allison on Immunotherapy
From Curiosity to Cure The latest episode of All Things Cancer features a powerful conversation with Nobel Laureate Dr. James Allison, whose work in immunotherapy has transformed cancer treatment across the globe. Hosted by Dr. Sujuan Ba, the episode dives into Dr. Allison’s early curiosity about the immune system, the years of resistance he faced from the scientific community, and the unforgettable moment when a patient’s tumors disappeared after receiving the drug he helped develop. More than a story of scientific discovery, it reminds us of the persistence, creativity, and support needed to turn bold ideas into life-saving treatments. Listen Now on Spotify | Apple Podcasts | and YouTube. About All Things Cancer Each episode of All Things Cancer will spotlight the most pressing topics in oncology, from cutting-edge treatments and emerging research to personal stories of resilience and hope. More than just a podcast, it’s a platform for raising awareness, advancing cancer education, and fostering a global community of support and collaboration. Hosted by NFCR CEO Sujuan Ba, Ph.D., this compelling series will bring together the entire ecosystem of cancer research—including leading scientists, oncologists, doctors, patient advocates, caregivers, biotech innovators, and survivors—for powerful discussions on the breakthroughs shaping the future of cancer research, treatment, and care. All Things Cancer is now available on Spotify and Apple Podcasts, with new episodes released biweekly. Stay up to date on the latest episodes and join the conversation that’s shaping the future of cancer research. Cancer impacts everyone—whether you're a patient, caregiver, advocate, or researcher, this podcast delivers invaluable insights from those on the frontlines of the fight against it. Sign-up to Be Informed When the Next Episode Comes Out!
Two NFCR-Supported Researchers Help Identify Cells That Naturally Fight Cancer
NFCR-supported researchers Dr. Suzanne Topalian of Johns Hopkins University and her collaborator Dr. Paul Nghiem of the University of Washington co-authored a study titled "A minimal gene set characterizes TIL specific for diverse tumor antigens across different cancer types" that was published in Nature Communications. The study identified a small group of key genes that help find special immune cells called tumor-infiltrating lymphocytes (TILs) that naturally fight cancer. These immune cells can recognize and attack different types of tumors, making them important for cancer treatment. Understanding which genes control these cells could help researchers develop better cancer therapies, especially immunotherapy, which boosts the body’s natural defenses against cancer. This discovery may lead to more effective ways to identify and activate the immune system to fight cancer. From Dr. Suzanne Topalian: Our continuing studies to profile T cells recognizing virus-positive vs virus-negative MCCs will build on these initial findings to provide an in-depth characterization of the immune response against MCCs. We anticipate that such work may lead to enhanced therapeutics and immune monitoring tools. Please know how much NFCR funding is appreciated in support of these investigations. Your support is making a difference in the fight against cancer! Donate today and be a part of the cure with NFCR. About Immunotherapy Cancer Immunotherapy is a groundbreaking new frontier in cancer treatment that helps empower patients’ own immune systems to recognize and attack cancer cells, providing new hope and critical treatment options for many patients with advanced cancers that were previously difficult to treat effectively. Learn More>>> Collaboration to Accelerate Discoveries With NFCR support, Dr. Nghiem and Dr. Topalian are collaborating to tackle the problem of why and how the body’s immune system sees virus-induced and UV light-induced MCC differently. Their studies of immune responses will help determine new combination therapies to save more patients from MCC. About Suzanne Topalian Dr. Suzanne Topalian is a physician-scientist whose studies of anti-tumor immunity have been foundational in developing cancer immunotherapy. Her research catalyzed the cancer community to develop the current FDA approval of 6 different checkpoint inhibitors (ICIs) for 17 types of cancer. About Paul Nghiem Dr. Paul Nghiem is a physician-scientist and leader in the research and treatment of Merkel cell carcinoma (MCC), a rare and deadly skin cancer. Studies by Dr. Nghiem’s team have resulted in the first two FDA-approved therapies for MCC. Sign-up to Stay Informed About Cancer Research Breakthroughs with NFCR!
NFCR-Supported Research Team Working On CAR-T Immunotherapy For Pancreatic Cancer
Pancreatic cancer is one of the most lethal malignancies with few treatment options. Its five-year survival rate is only about 10% in the US. Several treatment options are available for pancreatic cancers, including surgery, chemotherapy, radiation therapy, immunotherapy, and combinational therapies. However, these therapies are ineffective for most patients, and the outcomes are far from satisfactory. Current Immunotherapy Has Limited Effects on Pancreatic Cancer Immunotherapies hold great potential for several types of cancer, but they have limitations to pancreatic cancer. Antibody-based immunotherapy, such as the checkpoint inhibitor drug pembrolizumab, only works for a small portion (1-2%) of pancreatic patients who carry the genomic abnormalities called “mismatch repair-deficient (dMMR) or “microsatellite instability stability high” (MSI-H). T-cell-based immunotherapy, such as Chimeric Antigen Receptor (CAR) T-cell therapy or CAR-T therapy, has shown limited treatment effects on pancreatic cancer because it is difficult for T-cells to penetrate the tumors and kill them. Pancreatic Cancers are Often Called “Cold Tumors” Pancreatic cancers are “cold tumors” or “immune-excluded tumors” because the cancer-killing T-cells couldn’t efficiently infiltrate the tumor and only stay at the margins. Research data shows that pancreatic ductal adenocarcinoma (PDAC) builds up a surrounding microenvironment that suppresses the cancer-killing functions of the immune system. To turn the “cold tumor” into a “hot tumor,” researchers must explore novel approaches to disrupt the tumor-friendly microenvironment around the pancreatic tumors and enable more tumor-killing T-cells to infiltrate the tumor sites. Novel CAR-T Cells May Infiltrate Pancreatic Cancer More Efficiently Avery D. Posey, Jr., Ph.D. at the Center for Cellular Immunotherapy, University of Pennsylvania School of Medicine, is leading a research team to develop a novel type of CAR-T Cell therapy to overcome the limitation of current cell therapy procedures. Unlike antibody drugs, CAR-T therapy uses living cells to treat cancer in three steps. First, doctors collect the cancer-fighting T-cells from patients. Then, specialized technicians will modify those cells in the laboratory with genetic engineering technology. The engineered T-cells will be tailored to attack the patient’s tumor specifically. They are also armed with new genes, enabling them to penetrate tumors more efficiently than the patient’s natural T-cells. As the final step, modified CAR T-cells will be infused back into the patient to let them find and kill the cancer cells. How We Make An Impact With the NFCR’s support, Dr. Posey is collaborating with Dr. Courtney Houchen at the University of Oklahoma Health Sciences Center to conduct the research. They will make the novel CAR-T cells ready for human clinical trials after generating enough data in their laboratories. Learn more about Dr. Posey’s research project on the novel CAR-T Therapy by watching this video. References: CAR T Cells: Engineering Patients’ Immune Cells to Treat Their Cancers. National Cancer Institute, March 10, 2022.